Innovative Enhancements
The Olive team is dedicated to doing everything we can do to give you the best chance of a healthy pregnancy. In addition to IVF, we may recommend one or more innovative evidence-based reproductive technologies, depending on your diagnosis and treatment plan. These technologies can allow your doctor to tailor treatment more precisely to your unique fertility profile, thus increasing your chances of implantation, pregnancy and a healthy baby.

Choose a Service
Preimplantation Genetic Testing (PGT-M / PGT-SR)
Preimplantation genetic testing (PGT) is a method of testing embryos for specific genetic conditions to select the healthiest embryos for implantation.
If the genetic testing involves a single gene or monogenic condition, it is referred to as PGT-M (Preimplantation Genetic Testing for Monogenic Disorders). If the genetic condition involves a chromosome rearrangement such as a translocation or inversion, it is called PGT-SR (Preimplantation Genetic Testing for Structural Rearrangements).
PGT is indicated if you or your partner carry or are affected with a serious genetic disease like cystic fibrosis, fragile X syndrome, muscular dystrophy, Huntington disease and others, that may be passed on to your offspring. The purpose of PGT is to choose an embryo that is not affected by the disease.
We have a specialized PGT team at Olive, including Dr. Albert Yuzpe, Nora, our PGT Nurse Coordinator, and our Genetic Counsellors, Rachel, Colleen, and Sarah. As a first step, Dr. Yuzpe will meet with you to discuss the steps involved and review whether PGT may be an option, given your personal and family history. After this session, individuals or couples interested in pursuing PGT will have a session with one of our Genetic Counsellors. This session is designed to answer any questions about the current genetic issue, to review the steps involved at Olive in coordination with the US testing lab, and to explain the testing procedure and potential outcomes. The PGT nurse coordinator will be in touch to ensure there are no other fertility issues that need to be addressed, and to coordinate the IVF cycle.
PGT involves going through an IVF or ICSI cycle to obtain embryos which are subsequently biopsied in the laboratory. Depending on your situation, additional blood testing may be required for you and your partner. One or several cells from the embryo are sent to an expert genetic testing facility, and the results are obtained 2-3 weeks later. While waiting for the test results, your embryos will be flash frozen so that they are ready to transfer when the results are available, and the timing is right for your cycle. The results of the genetic testing will be discussed with you by Dr. Yuzpe or one of the Genetic Counsellors.
The diagnostic accuracy of PGT is between 90-99% when looking for a known genetic condition. However, the chances of a successful pregnancy will depend on multiple factors, including your age, hormone profile, and history. Your physician at Olive will review these details with you.
Ask your GP or walk-in clinic for a referral to Olive. Your Olive physician will review the details and help you get started.
Next: Preimplantation Genetic Testing for Aneuploidy (PGT-A)
Preimplantation Genetic Testing for Aneuploidy (PGT-A)
Preimplantation genetic testing for aneuploidy (PGT-A) is a screening technique used with IVF that identifies chromosomally healthy (euploid) embryos for transfer during an IVF procedure. Most miscarriages are due to abnormal (aneuploid) embryos.
Selecting embryos that have been identified as normal with PGT-A can
-
Increase pregnancy rates to 70% or more.
-
Reduce miscarriage rates to 5%-7%.
-
Minimize risks for chromosomal anomalies.
-
Allow chromosomally normal embryos to be frozen for future use.
PGT-A can increase the chance of a healthy pregnancy for anyone having IVF, but you may particularly want to consider it if you have had repeated miscarriages, failed IVF, or are over 36 years of age.
Typically, in IVF embryos are graded by their appearance. However, this is a bit like “judging a book by its cover” as there is no way of determining whether an embryo has the right number of chromosomes based on its appearance. PGT-A lets us verify that embryos appearing normal are in fact chromosomally normal.
Embryos created by IVF are grown up to the blastocyst stage (5 or 6 days after fertilization). A sample of about 5-10 cells are biopsied from the portion of the embryo destined to form the placenta. The inner cell mass, which will eventually form the baby, is not touched.
The embryos are frozen and remain at Olive, but cells are sent to a laboratory for genetic testing. The number of chromosomes for each embryo is analyzed with a technique called next-generation sequencing (NGS).
Step 1
Mature eggs are removed from the ovary.
Step 2
The eggs are fertilized in the lab.

Step 3
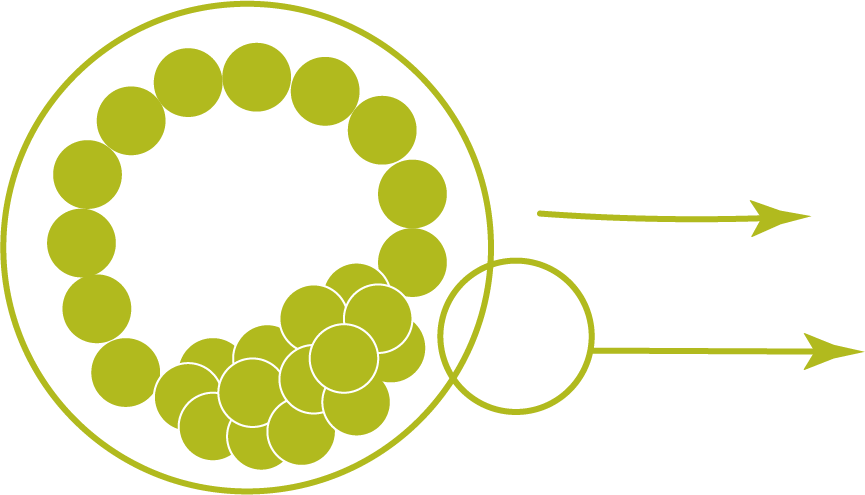
Embryo cells divide.
Step 4
A blastocyst is biopsied at day 5, 6 or 7.

Step 5
DNA of 5-10 cells from the placental area are examined. Test results are returned within 10-14 days.
Step 6
Chromosomally healthy embryos are frozen for future transfer into the uterus.
Results will be relayed to you by a telephone call from one of the clinic doctors or genetic counselors. Details of the results for each embryo tested will be reviewed with you at this time and may include the following outcomes:
- Normal chromosome number (euploid): These embryos have 46 chromosomes in each cell and are the best candidates for a successful transfer.
- Abnormal chromosome number (aneuploid): These embryos have missing or extra whole or partial chromosomes in every cell and are likely to result in a miscarriage, failed transfer, or a baby with a chromosomal disorder like Down syndrome. The probabilities of these outcomes increase with maternal age.
- Mosaicism: Embryos with a mosaic finding have some cells with a normal number of chromosomes and some cells with extra or missing whole or partial chromosomes. This result is less clear than the first two outcomes. There are a number of different options and your physician and/or the genetic counselling team will consult with you and advise on what to do in your case.
This result is less clear than the first two options.
Mosaic embryos with chromosomal abnormalities associated with known genetic syndromes, such as trisomy 21,13,18, are not recommended for transfer
Transferring any mosaic embryo is associated with uncertainty as to the possible health of the child
Whether you keep, discard, or use mosaic embryos is decided after consultation with your physician and/or genetic counselling team
- Failed QC metrics or No Diagnosis: Results were unable to be obtained due to several possible issues. This occurs in about 2% of biopsies. Embryo rebiopsy is offered at no charge.
As PGT-A requires several additional steps compared to traditional IVF, there is an increase in cost. However, many experts believe that the overall advantages of PGT-A, such as improved pregnancy rates and decreased miscarriage rates, will result in an overall cost benefit. It is also worth considering if you would like more than one child, as you can have assurance of stored healthy embryos to implant at a later date.
The Olive finance department will discuss the expenses in detail.
Book an appointment to learn more about whether PGT-A is right for you.
Next: Endometrial Receptivity Array (ERA)
Endometrial Receptivity Array (ERA)
In most cases where an embryo does not implant, it is because it has an abnormal number of chromosomes. However, there is a percentage of apparently “normal” embryos that fail to implant. This suggests that the uterine environment may be a factor in the success of an embryo transfer. Olive offers additional testing of the uterine environment to potentially identify optimum treatment before embryo transfer.
ERA is a test that helps identify more precisely when your endometrium (lining of the uterus) is receptive to implantation by an embryo. Endometrial receptivity is the time sensitive window for implantation (WOI). Most patients will have a similar WOI, but some will fall outside the typical time frames with the result that the embryo fails to implant.
The ERA test involves taking a few endometrial cells at certain times in your cycle and analyzing whether they are receptive or non receptive and whether your WOI is open. By identifying your specific WOI your doctor can create a unique, personalized embryo transfer protocol (pET).
You should discuss the ERA test with your fertility doctor if:
- You have had 2 or more unsuccessful embryo transfers with high quality untested embryos
- You have had 1 or more unsuccessful embryo transfers after PGT-A
- You have had concerns with endometrial lining (example: thin endometrial lining)
A study* conducted by the medical team at Olive Fertility Centre found implantation and ongoing pregnancy rates were higher (73.7 vs. 54.2% and 63.2 vs. 41.7%, respectively) for patients receiving pET compared to patients without pET. It also found that using a modified progesterone protocol may improve the outcomes of subsequent healthy frozen embryo transfers.
* Tan J, Kan A, Hitkari J, Taylor B, Tallon N, Warraich G, Yuzpe A, Nakhuda G. The role of the endometrial receptivity array (ERA) in patients who have failed euploid embryo transfers. J Assist Reprod Genet. 2018 Apr;35(4):683-692. doi: 10.1007/s10815-017-1112-2. Epub 2018 Jan 11. PMID: 29327111; PMCID: PMC5949105. https://pubmed.ncbi.nlm.nih.gov/29327111/
Next: Tests for Assessing the Uterine Microbiome
Tests for Assessing the Uterine Microbiome
You may have heard a lot recently about the microbiome and gut health (the microbiome is the environment within our bodies composed of trillions of other living organisms including bacteria, archaea, fungi and viruses). Increasingly highly sensitive technologies like next generation sequencing are showing that your microbiome affects fertility as well. Internal and external factors may cause microbial imbalances (dysbiosis) in the lower and/or upper reproductive system which can result in infertility or failure of the embryo to implant or miscarriage.
EndomeTRIO is a complete endometrial analysis that includes ERA (described above), EMMA and ALICE tests described below.
EMMA (Endometrial Microbiome Metagenomic Analysis)
Dysbiosis of the uterine cavity has been associated with poor reproductive outcomes in IVF patients, suggesting that deviations of the Lactobacillus endometrial content could play a role in infertility. EMMA is a screening test that quantifies the abundance of healthy bacteria (Lactobacillus) in your endometrium.
EMMA assesses the balance of the microbiome and can reveal a low biomass or a reduced concentration of the healthy bacteria, which can then lead to the healthy bacteria being overrun by the troublemakers. According to one study*, the presence of a non-Lactobacillus-dominated microbiota in a receptive endometrium was associated with significant decreases in implantation, pregnancy, ongoing pregnancy and live birth rates.
* Moreno I, Codoñer FM, Vilella F, Valbuena D, Martinez-Blanch JF, Jimenez-Almazán J, Alonso R, Alamá P, Remohí J, Pellicer A, Ramon D, Simon C. Evidence that the endometrial microbiota has an effect on implantation success or failure. Am J Obstet Gynecol. 2016 Dec;215(6):684-703. doi: 10.1016/j.ajog.2016.09.075. Epub 2016 Oct 4. PMID: 27717732.
Who Should Consider EMMA?
Emma can be beneficial for patients who have experienced repeated implantation failure.
ALICE (Analysis of Infectious Chronic Endometritis)
ALICE detects the presence of unhealthy flora that causes chronic endometritis (CE)--a low-level infection that causes persistent inflammation of the endometrial lining--and recommends antibiotic and probiotic treatment. Although CE does not usually cause any noticeable symptoms, it is linked** to an up to 42% implantation failure and recurrent miscarriage.
** (Moreno I, Cicinelli E, Garcia-Grau I, Gonzalez-Monfort M, Bau D, Vilella F, De Ziegler D, Resta L, Valbuena D, Simon C. The diagnosis of chronic endometritis in infertile asymptomatic women: a comparative study of histology, microbial cultures, hysteroscopy, and molecular microbiology. Am J Obstet Gynecol. 2018 Jun;218(6):602.e1-602.e16. doi: 10.1016/j.ajog.2018.02.012. Epub 2018 Feb 23. PMID: 29477653)
Who Should Consider ALICE?
ALICE can be beneficial for anyone wishing to conceive or who has a history of failed implantation and repeated pregnancy loss.
Learn More about this Topic
Olive clinic experts have shared helpful insights on the Olive blog. Check out the following quick reads to learn more.

